Malignancy mimicker of the treated breast and MR imaging
- Posted by Mirror Organization
- Categories Diagnostic, Mammogram Cases, Modality, MRI Cases
- Date September 27, 2020
- Comments 0 comment
Author / Copyright: Dr.Carmen Ali (Port-Saied University)
Clinical History
Female patient aged 51 years old with history of left breast invasive lobular carcinoma. The patient underwent conservative quadrantectomy and she has undergone routine follow up.
Case Imaging Scenario
On follow up digital mammography and breast ultrasound were done and there was an area of focal asymmetry in the operative bed of the left breast with skin thickening and mild parenchymal edema.
According to the digital mammography and breast ultrasound findings, the patient was categorized according to Breast Imaging Reporting and Data System as BI-RADS 4a. Biopsy and further evaluation by MRI were recommended.
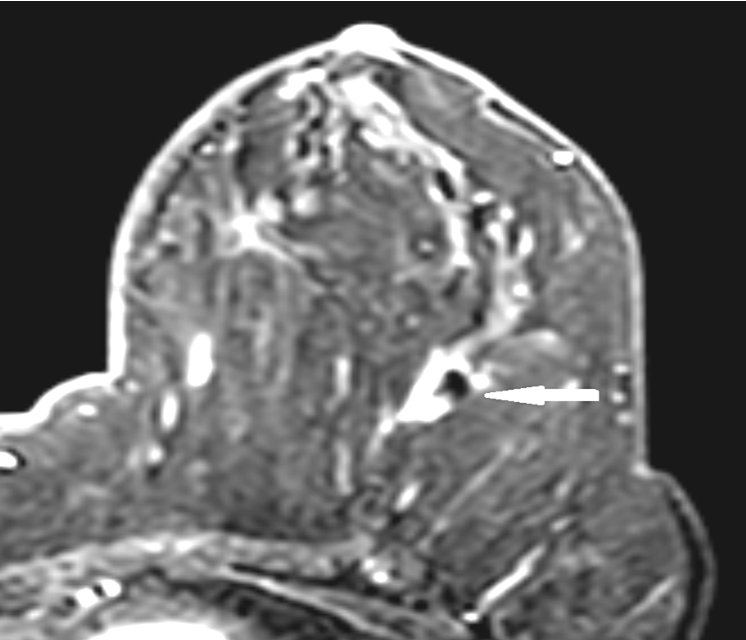
The patient performed dynamic post contrast breast MRI with diffusion. Axial T1 non fat saturated sequence was evaluated first and there was well circumscribed rounded high signal lesion in the operative bed corresponding to the site of focal asymmetry previously described by digital mammography (Figure 1). The lesion showed a low signal in short T1 inversion recovery (STIR) techniques denoting its fatty nature (Figure 2).
In post contrast study the lesion showed thick smooth rim enhancement (Figure 3). The enhancing rim of the lesion showed slow initial rise and type II plateau time/signal intensity curve (Figure 4).
In diffusion images the lesion showed free diffusion with high apparent diffusion coefficient (ADC) value in ADC map (Figure 5 & 6).
According to the post contrast MRI findings and diffusion behaviour, the lesion was categorized as BI-RADS 3 and it was reported as fatty lesion mostly postoperative fat necrosis surrounded by non-enhancing fibrous scar.





Fat necrosis is a common benign lesion of the breast. It is resulting from necrosis of the fat cells as result of a vascular ischemia. It is usually related to blunt trauma, previous biopsy, lumpectomy, reduction mammoplasty or radiation therapy [1].
In postoperative breast the presence of architectural distortion, post-treatment edema and increased breast density in digital mammography and breast ultrasound may impair detection of postoperative malignant recurrence [2].
Post contrast MRI of breast has an important role in evaluation of the postoperative breast lesions, like distortion that seen in mammographic follow up of the post-operative breast [3].
The diagnosis of postoperative fat necrosis is considered as a challenging imaging pitfall. Once fat necrosis is diagnosed it is categorized as BI-RADS 2 or BI-RADS 3 category.
In post contrast breast MRI the margins and the enhancement pattern of fat necrosis may be indistinguishable from recurrent malignant tumor. The clue for the diagnosis of postoperative fat necrosis in breast MRI is the presence of fat on T1WI [4].
The patient performed breast MRI and there was a lesion in the operative bed of the left breast. In non-fat saturated T1 images the fat within the lesion had the same signal of the surrounding breast parenchymal fat and it was surrounded by a hypointense area of architectural distortion. In short T1 inversion recovery (STIR) images the fat within the lesion was low signal like the normal surrounding parenchymal fat.
After post contrast study the fatty lesion showed homogeneous thick rim enhancement and this was in agreement with the commonest enhancing pattern of fat necrosis reported by Daly et.al. [1]. The architectural distortion area surrounding the lesion showed no significant enhancement in post contrast study and this excludes the presence of post-operative malignant residual or recurrence.
The time signal intensity curve of the enhancing part of the lesion showed slow rise in early phase with plateau delayed phase (type II borderline plateau curve). This pattern was reported by Chala et.al. he noted that fat necrosis enhancement patterns may be similar to those seen in malignant lesions and the degree of this enhancement depends on the degree of the associated inflammatory process [5].
In diffusion weighted images (DWI) the lesion and its surrounding architectural distortion showed free diffusion with high apparent diffusion coffiecient (ADC) value denoting its benign nature and this match with Mansour et.al. study they concluded that MR diffusion increases the MRI diagnostic value in differentiation between postoperative benign and malignant breast lesions [6].
Teaching Points:
- Fat and non fat saturated MRI sequences have great ability for diagnosis of post-operative breast fatty lesions.
- Post-contrast MRI could be misleading due to overlap between benign postoperative changes and postoperative residual or recurrence.
- Diffusion imaging supported by ADC values could differentiate between benign and malignant post-operative breast sequelae.
Final Diagnosis:
Postoperative fat necrosis of left breast surrounded by fibrotic scar tissue.
Differential Diagnosis List:
Post-operative malignant recurrence.
Post-operative inflammation.
Keywords:
Post-operative; fat necrosis; breast MRI; recurrent cancer.
- Daly CP, Jaeger B and Sill DS. Variable Appearances of fat necrosis on breast MRI. AJR. (2008) 191:1374–1380.
- EL-Adalany AI and Hamed EE. Role of dynamic contrast enhanced MRI in evaluation of post-operative breast lesions. EJRN (2016) 47, 631–640.
- Devon RK, Rosen MA, Mies C, et al. Breast reconstruction with a transverse rectus abdominis myocutaneous flap: spectrum of normal and abnormal MR imaging findings. Radiographics (2004);24:1287–99.
- Drukteinis JS, Gombos EC, Raza S, et al. MR imaging assessment of the breast after breast conservation therapy: distinguishing benign from malignant lesions. Radiographics (2012);32:219–34.
- Chala LF, Barros ND, Camargo PD, Endo E, Kim SJ, Pincerato MK et. al. Fat Necrosis of the Breast: Mammographic, Sonographic, Computed Tomography, and Magnetic Resonance Imaging Findings. Curr Probl Diagn Radiol. (2004). 106-126.
- Mansour SM and Bahiry N. Residual breast cancer or postoperative changes: Can Diffusion-weighted magnetic resonance imaging solve the case? EJRN.(2015). 46.225-234.
The imaging investigations were performed at Mansoura university hospitals

